Search Results
video (7)
General Considerations for the Placement of Renal Stents
videoIntroduction The use of renal stents in atherosclerotic renal artery stenosis has been mired in controversy secondary to poorly designed randomized clinical trials which demonstrated minimal benefit over medical management. This publication illustrates the deployment of an isolated renal stent as an ancillary procedure for a patient with a 5.5cm juxtarenal AAA in need of fenestrated endovascular repair. Methods Under general anesthesia, the patient was prepped with the left arm tucked. Access via the right common femoral artery over the femoral head was obtained under ultrasound guidance. Using the Seldinger technique, a long sheath (Ansell) was inserted to the level of the infrarenal aorta. A Glidewire (Terumo) was used to enter the right renal ostia with the assistance of an Omniflush (Angiodynamics) catheter after an initial aortogram. A Rosen (Cook) wire was exchanged and the sheath was advanced past the stenosis over the dilator. The balloon mounted iCAST (Atrium) stent was positioned and the sheath pulled back. The stent was deployed and flared using a Flash ostial balloon (Cordis). Completion angiography demonstrated excellent flow through the right renal artery and into the terminal renal branches. Results The patient recovered uneventfully overnight with a stable Cr the next morning. Four weeks after his renal intervention, the patient was taken to the operating theatre for a successful 3-vessel fenestrated aortic repair. At the most recent 6-month follow-up, the patient had a stable Cr and residual aortic sac diameter. Conclusions While the use of renal stenting in hypertension related to atherosclerotic renal artery disease continues to remain controversial, this intervention can still be performed as an adjunctive procedure in select cases with excellent technical success and low morbidity. Additional Authors Raghu L. Motaganahalli Andres Fajardo
A Guide to Temporal Bone Dissection: Cortical Mastoidectomy & Facial Recess Approach (Part 1 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Description This video covers the key steps of a cortical mastoidectomy and facial recess approach during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. The first part of this video demonstrates a basic cortical mastoidectomy and focuses on fundamental principles including the preservation of the tegmen and sigmoid plate, adequate posterior canal wall thinning, continual saucerization, adequate removal of air cells, and early identification of the lateral semicircular canal and incus. The second part of the video discusses the facial recess approach and enlightens the viewer on the boundaries of the facial recess, the course of the mastoid segment of the facial nerve, and the location of the round window. Key surgical landmarks demonstrated in the course of this video include: zygomatic root, temporal line, posterior meatal wall, Henle’s spine, mastoid tip, tegmen mastoideum, sigmoid sinus, Koerner’s septum, lateral semicircular canal, incus, incus buttress, chorda tympani nerve, mastoid segment of the facial nerve, facial recess, round window niche, and round window.
A Guide to Temporal Bone Dissection: Endolymphatic Sac Dissection (Part 2 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video shows the key steps in the dissection of the endolymphatic sac during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part one of our video series and demonstrates fundamentals of endolymphatic surgery including the location and appearance of the endolymphatic sac, and its relationship to the labyrinth. Key surgical landmarks demonstrated in the course of this video include: sigmoid sinus, mastoid segment of the facial nerve, retrofacial air cells, endolymphatic sac, lateral and posterior semicircular canal, and Donaldson’s line
A Guide to Temporal Bone Dissection: Lateral Temporal Bone Resection (Part 3 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video covers the key steps of a lateral temporal bone resection during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part two of our video series. This approach allows for the en bloc removal of the external auditory canal and demonstrates fundamental steps of the procedure including: the propagation of a superior trough between the tegmen and the superior aspect of the external auditory canal, the extension of the facial recess inferiorly with sacrifice of the chorda tympani, and the drilling of the hypotympanic bone towards the glenoid. At the completion of the demonstration, the viewer is afforded a labelled view of the medial wall of the mesotympanum, as well as the medial aspect of the external auditory canal with an intact tympanic membrane. Key surgical landmarks demonstrated in the course of this video include: tegmen, zygomatic root, malleus, incus, stapes, glenoid, eustachian tube, mastoid segment of the facial nerve, chorda tympani nerve, facial recess, hypotympanic space, annular bone, tensor tympani tendon, cochlear promontory, pyramidal process, round window, and lateral semicircular canal.
A Guide to Temporal Bone Dissection: Labyrinthectomy (Part 4 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video demonstrates the key steps of a labyrinthectomy during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part three of our video series and demonstrates fundamental steps involved in a labyrinthectomy including: the identification of the three-dimensional (3D) orientation of the semicircular canals, the location of the common crus, the relationship between the second genu of the facial nerve and the posterior semicircular canal, the relationship of the vestibule to the endolymphatic sac, the course of the subarcuate artery, and the relationship of the labyrinth to the internal auditory canal. Key surgical landmarks demonstrated in the course of this video include: posterior semicircular canal, superior semicircular canal, lateral semicircular canal, common crus, external genu of facial nerve, tympanic segment of the facial nerve, tegmen, vestibule, endolymphatic sac, endolymphatic duct, subarcuate artery.
A Guide to Temporal Bone Dissection: Internal Auditory Canal Dissection (Part 5 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video demonstrates key steps in the dissection of the internal auditory canal during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part four of our video series and demonstrates fundamental steps involved in the dissection of the internal auditory canal including: establishing an inferior trough and identification of the cochlear aqueduct, establishing a superior trough and identification of the labyrinthine segment of the facial nerve, and blue-lining the internal auditory canal from porous to fundus. Key surgical landmarks demonstrated in the course of this video include: internal auditory canal, cochlear aqueduct, meatal segment of the facial nerve, labyrinthine segment of the facial nerve, 1st genu of the facial nerve, tympanic segment of the facial nerve, 2nd genu of the facial nerve, mastoid segment of the facial nerve.
A Guide to Temporal Bone Dissection: Infratemporal Approach (Part 6 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video demonstrates key steps in the infratemporal approach during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part five of our video series and demonstrates fundamental steps of the procedure including: decompression and mobilization of the facial nerve, dissection of the cochlear scalae, skeletonization of the carotid artery, and entry into the jugular bulb. We demonstrate the wide opening of the jugular bulb to facilitate visualization of the medial wall of the jugular bulb, which subsequently aids in the dissection of the pars nervosa. Key surgical landmarks demonstrated in the course of this video include: sigmoid sinus, jugular bulb, mastoid segment of the facial nerve, cochlear scalae, internal carotid artery, pars nervosa
webinar (1)
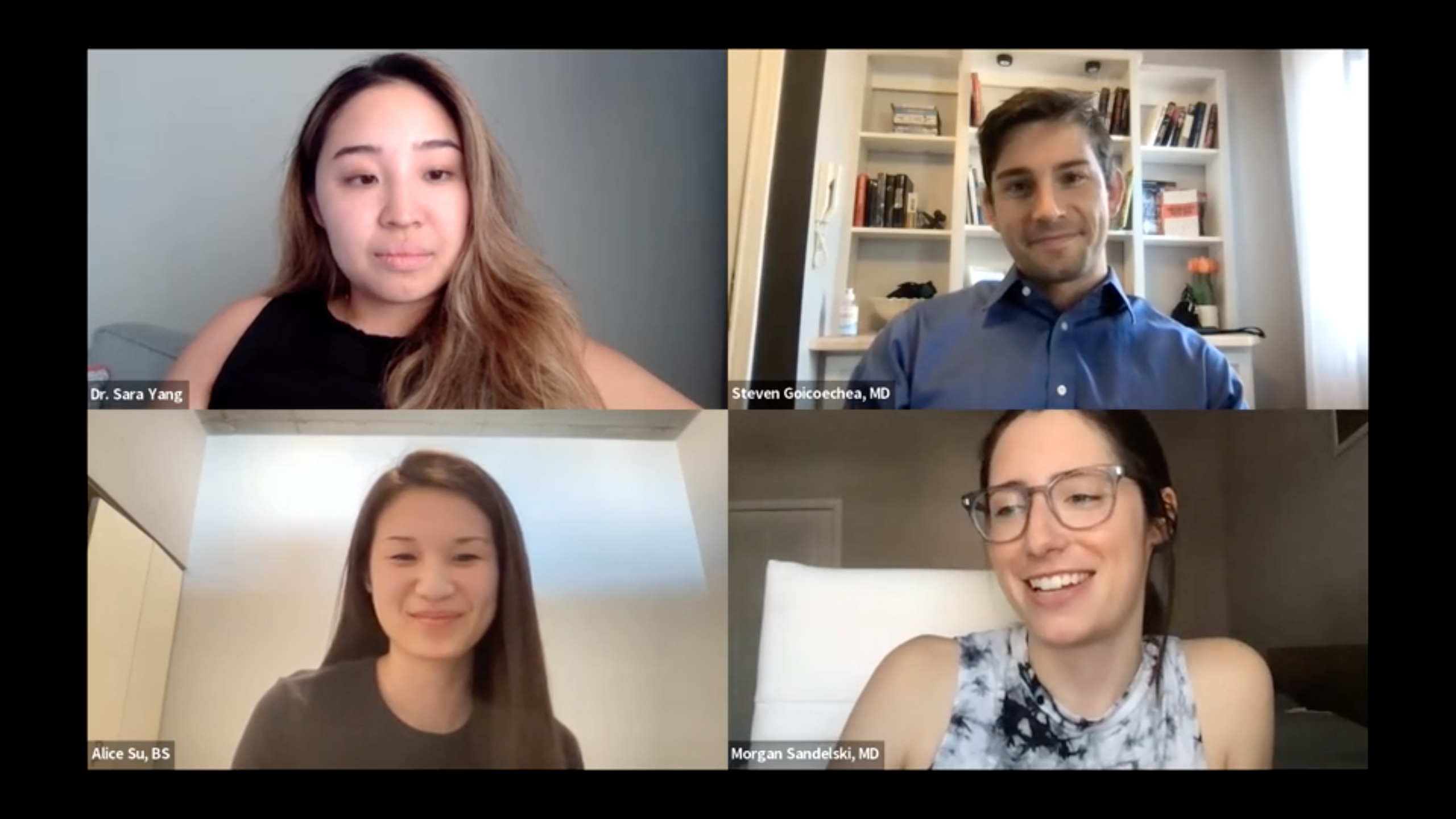
What is Otolaryngology: More than Tonsils and Boogers
webinar
Come learn more about the jobs of Otolaryngologists (also known as ENT doctors!). We will discuss the breadth and depth of what ENT doctors cover with case descriptions. Medical students and residents of different levels will be on a panel to answer questions about the journey to and through Otolaryngology residency.

Otolaryngology Head and Neck Surgery / Resident Physician, PGY 5
Loyola University Medical Center
Dr Yang grew up in the arid and desert like climate of Eastern Washington before spending four years in rainy Seattle during her undergrad years, majoring in Neurobiology at the University of Washington. She then moved to sunny Southern California to complete her medical education at Loma Linda University School of Medicine. She is currently finishing her chief year of Otolaryngology Head and Neck Surgery residency at Loyola University Medical Center in Chicago, enjoying both life in the Windy City and surviving the cold winters. She recently matched to fellowship at Oregon Health and Science University in Facial Plastics and Reconstruction with Dr. Wax to specialize in microvascular reconstruction of complex head and neck defects. She is excited to return to the west coast and explore all the nature that Oregon has to offer.

Resident physician
University of Nebraska Medical Center
Steven is originally from San Diego, CA and attended the University of Notre Dame where he studied anthropology. He then earned a master's degree at Boston University and completed a year of service with Jesuit Volunteer Corps Northwest in Yakima, WA. Steven recently graduated from Loyola University Chicago Stritch School of Medicine and will be starting otolaryngology residency at the University of Nebraska Medical Center.
Medical Student
Loyola University Chicago Stritch School of Medicine
Alice is originally from San Jose, CA and attended UC Berkeley where she studied Molecular and Cell Biology as well as Nutrition. She is starting her fourth year at Loyola University Chicago Stritch School of Medicine, and preparing to apply for otolaryngology residency.

Resident
Loyola University Medical Center Otolaryngology Head and Neck Surgery Department
Dr. Sandelski grew up in Northwest Indiana, leaving the state for undergrad at the University of Michigan, and returning for medical school at Indiana University School of Medicine. She is in her second year at Loyola for ENT residency. She is undecided for plans after residency, with current interests in head and neck oncology and facial plastics and reconstruction.