Search Results
We found 24 results for India in video, leadership, management, webinar, news & Other
video (11)
Laparoscopic Adrenalectomy
videoLaparoscopic adrenalectomy (LA) was first described by Gagner et al. in the early 1990s, and has since become the gold standard for removal of small and medium sized adrenal tumors. Most commonly, LA is performed for unilateral benign adrenal lesions, however the minimally invasive technique is also routinely used for bilateral disease, as well as myelolipomas, adrenal cysts, adrenal hemorrhage and androgen-secreting tumors. Compared with the open approach, LA offers shorter hospital stay, improved patient satisfaction, decrease post-operative pain and markedly improved cosmesis. Even more, the difficulty in obtaining adequate open surgical exposure, combined with the diminutive size of the adrenal gland make laparoscopy an especially attractive option. Given this, we decided to proceed with LA approach for our patient who presented with NSCLC metastasis to his right adrenal. DOI# http://dx.doi.org/10.17797/4ek02iupxd Mellon MJ, Sethi A, Sundaram CP. Laparoscopic adrenalectomy: Surgical techniques. Indian Journal of Urology : IJU : Journal of the Urological Society of India. 2008;24(4):583-589. doi:10.4103/0970-1591.44277. Gagner M, Lacroix A, Bolte E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. N Engl J Med. 1992;327:1033.
General Considerations for the Placement of Renal Stents
videoIntroduction The use of renal stents in atherosclerotic renal artery stenosis has been mired in controversy secondary to poorly designed randomized clinical trials which demonstrated minimal benefit over medical management. This publication illustrates the deployment of an isolated renal stent as an ancillary procedure for a patient with a 5.5cm juxtarenal AAA in need of fenestrated endovascular repair. Methods Under general anesthesia, the patient was prepped with the left arm tucked. Access via the right common femoral artery over the femoral head was obtained under ultrasound guidance. Using the Seldinger technique, a long sheath (Ansell) was inserted to the level of the infrarenal aorta. A Glidewire (Terumo) was used to enter the right renal ostia with the assistance of an Omniflush (Angiodynamics) catheter after an initial aortogram. A Rosen (Cook) wire was exchanged and the sheath was advanced past the stenosis over the dilator. The balloon mounted iCAST (Atrium) stent was positioned and the sheath pulled back. The stent was deployed and flared using a Flash ostial balloon (Cordis). Completion angiography demonstrated excellent flow through the right renal artery and into the terminal renal branches. Results The patient recovered uneventfully overnight with a stable Cr the next morning. Four weeks after his renal intervention, the patient was taken to the operating theatre for a successful 3-vessel fenestrated aortic repair. At the most recent 6-month follow-up, the patient had a stable Cr and residual aortic sac diameter. Conclusions While the use of renal stenting in hypertension related to atherosclerotic renal artery disease continues to remain controversial, this intervention can still be performed as an adjunctive procedure in select cases with excellent technical success and low morbidity. Additional Authors Raghu L. Motaganahalli Andres Fajardo
A Guide to Temporal Bone Dissection: Cortical Mastoidectomy & Facial Recess Approach (Part 1 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Description This video covers the key steps of a cortical mastoidectomy and facial recess approach during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. The first part of this video demonstrates a basic cortical mastoidectomy and focuses on fundamental principles including the preservation of the tegmen and sigmoid plate, adequate posterior canal wall thinning, continual saucerization, adequate removal of air cells, and early identification of the lateral semicircular canal and incus. The second part of the video discusses the facial recess approach and enlightens the viewer on the boundaries of the facial recess, the course of the mastoid segment of the facial nerve, and the location of the round window. Key surgical landmarks demonstrated in the course of this video include: zygomatic root, temporal line, posterior meatal wall, Henle’s spine, mastoid tip, tegmen mastoideum, sigmoid sinus, Koerner’s septum, lateral semicircular canal, incus, incus buttress, chorda tympani nerve, mastoid segment of the facial nerve, facial recess, round window niche, and round window.
A Guide to Temporal Bone Dissection: Endolymphatic Sac Dissection (Part 2 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video shows the key steps in the dissection of the endolymphatic sac during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part one of our video series and demonstrates fundamentals of endolymphatic surgery including the location and appearance of the endolymphatic sac, and its relationship to the labyrinth. Key surgical landmarks demonstrated in the course of this video include: sigmoid sinus, mastoid segment of the facial nerve, retrofacial air cells, endolymphatic sac, lateral and posterior semicircular canal, and Donaldson’s line
A Guide to Temporal Bone Dissection: Lateral Temporal Bone Resection (Part 3 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video covers the key steps of a lateral temporal bone resection during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part two of our video series. This approach allows for the en bloc removal of the external auditory canal and demonstrates fundamental steps of the procedure including: the propagation of a superior trough between the tegmen and the superior aspect of the external auditory canal, the extension of the facial recess inferiorly with sacrifice of the chorda tympani, and the drilling of the hypotympanic bone towards the glenoid. At the completion of the demonstration, the viewer is afforded a labelled view of the medial wall of the mesotympanum, as well as the medial aspect of the external auditory canal with an intact tympanic membrane. Key surgical landmarks demonstrated in the course of this video include: tegmen, zygomatic root, malleus, incus, stapes, glenoid, eustachian tube, mastoid segment of the facial nerve, chorda tympani nerve, facial recess, hypotympanic space, annular bone, tensor tympani tendon, cochlear promontory, pyramidal process, round window, and lateral semicircular canal.
A Guide to Temporal Bone Dissection: Labyrinthectomy (Part 4 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video demonstrates the key steps of a labyrinthectomy during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part three of our video series and demonstrates fundamental steps involved in a labyrinthectomy including: the identification of the three-dimensional (3D) orientation of the semicircular canals, the location of the common crus, the relationship between the second genu of the facial nerve and the posterior semicircular canal, the relationship of the vestibule to the endolymphatic sac, the course of the subarcuate artery, and the relationship of the labyrinth to the internal auditory canal. Key surgical landmarks demonstrated in the course of this video include: posterior semicircular canal, superior semicircular canal, lateral semicircular canal, common crus, external genu of facial nerve, tympanic segment of the facial nerve, tegmen, vestibule, endolymphatic sac, endolymphatic duct, subarcuate artery.
A Guide to Temporal Bone Dissection: Internal Auditory Canal Dissection (Part 5 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video demonstrates key steps in the dissection of the internal auditory canal during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part four of our video series and demonstrates fundamental steps involved in the dissection of the internal auditory canal including: establishing an inferior trough and identification of the cochlear aqueduct, establishing a superior trough and identification of the labyrinthine segment of the facial nerve, and blue-lining the internal auditory canal from porous to fundus. Key surgical landmarks demonstrated in the course of this video include: internal auditory canal, cochlear aqueduct, meatal segment of the facial nerve, labyrinthine segment of the facial nerve, 1st genu of the facial nerve, tympanic segment of the facial nerve, 2nd genu of the facial nerve, mastoid segment of the facial nerve.
A Guide to Temporal Bone Dissection: Infratemporal Approach (Part 6 of 6)
videoAuthors Mohamedkazim M. Alwani, MD1, 3 Jon L. Harper, BS1, 3 Rick F. Nelson, MD PhD1, 2, 3 Author Affiliations Department of Otolaryngology – Head and Neck Surgery1 Department of Neurological Surgery2 Indiana University School of Medicine3 Video Description This video demonstrates key steps in the infratemporal approach during lab dissection of the temporal bone. The goal of this video is to serve as a supplementary teaching resource for resident-level surgical trainees by demonstrating key surgical landmarks and proper lab dissection technique. This video builds on part five of our video series and demonstrates fundamental steps of the procedure including: decompression and mobilization of the facial nerve, dissection of the cochlear scalae, skeletonization of the carotid artery, and entry into the jugular bulb. We demonstrate the wide opening of the jugular bulb to facilitate visualization of the medial wall of the jugular bulb, which subsequently aids in the dissection of the pars nervosa. Key surgical landmarks demonstrated in the course of this video include: sigmoid sinus, jugular bulb, mastoid segment of the facial nerve, cochlear scalae, internal carotid artery, pars nervosa
TENT TECHNIQUE OF LAPAROSCOPIC RETROPERITONEAL LYMPHADENECTOMY- TRANSPERITONEAL APPROACH
videoAuthors: First author: Dr. Thammineedi Subramanyeshwar Rao, M.S, MCh, FMAS Corresponding author: Dr. R Rajagopalan Iyer, DNB,FSOG,MNAMS,FMAS Third author: Dr. Srijan Shukla, M.S,FMAS Affiliation of all authors: Basavatarakam Indo-American Cancer Institute and Research Centre, Road no. 10, Banjara Hills, Hyderabad, Telangana, India; PIN: 500034 Corresponding author’s mailing address: Department of Surgical Oncology, 4th floor, Block 1, Basavatarakam Indo American Cancer Hospital, Road no. 10, Banjara Hills, Hyderabad, Telangana, India; PIN: 500034 Corresponding author's email address: rajagopalan99@hotmail.com Disclosure/ Conflict of interest: The authors whose names are listed above certify that they have NO affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers ’bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. NO FUNDING SOURCES .
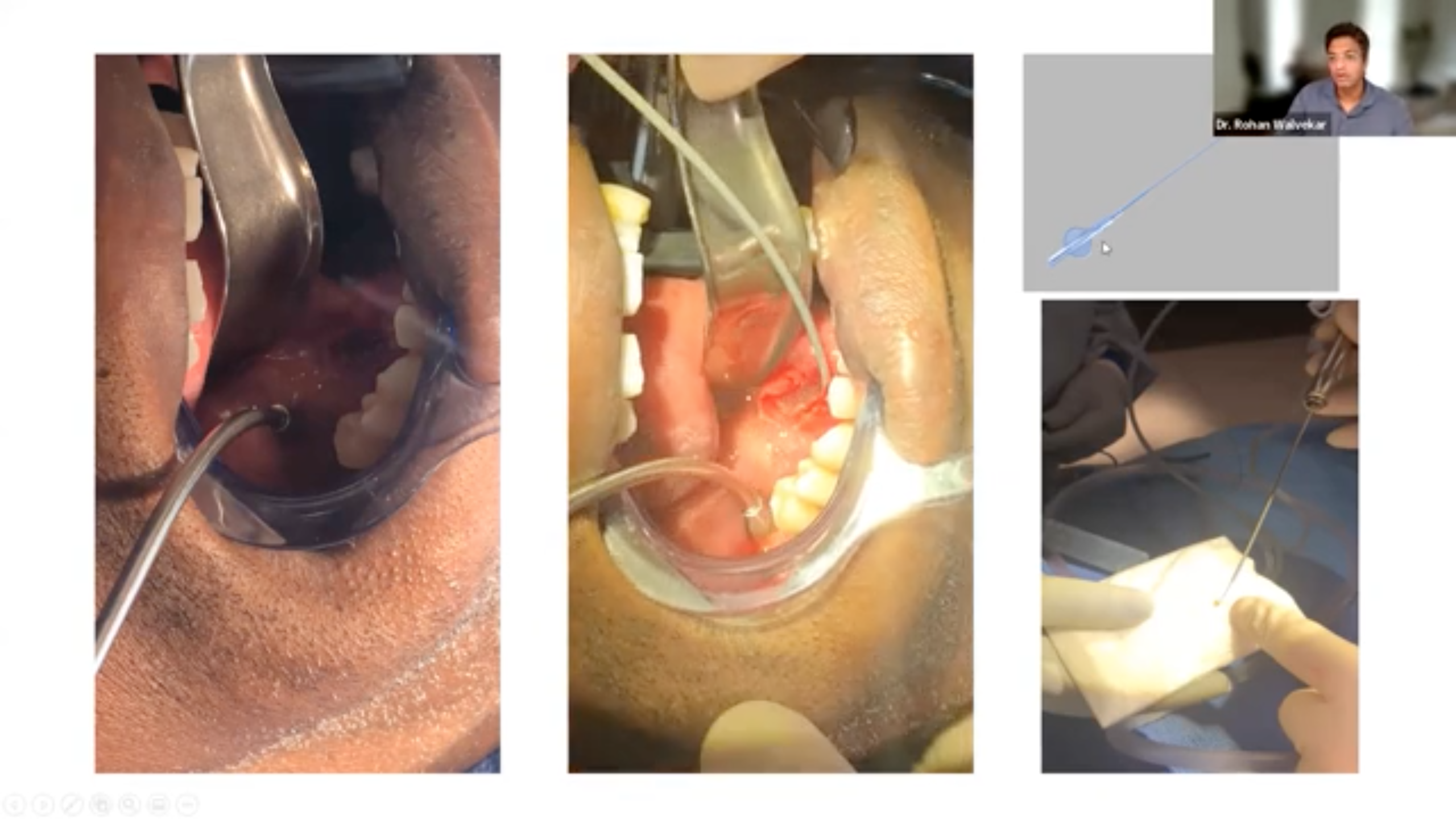
Nasopharyngeal Papillomatosis- A combined Transnasal Transoral Coblation Assisted Approach
videoTitle: Nasopharyngeal Papillomatosis- A combined trans nasal transoral coblation assisted approach Authors - 1. Dr Deepa Shivnani- corresponding author MBBS, DNB Otolaryngology , MNAMS, Fellowship in Pediatric Otolaryngology Children’s Airway & Swallowing Center Manipal Hospital, Bangalore , India email- deepa.shivnani14@gmail.com 2. Dr E V Raman MBBS, DLO , MS Otorhinolaryngology Children’s Airway & Swallowing Center Manipal Hospital, Bangalore Here I am presenting a case of 16 yrs old boy, who had nasal block and occasional cough. Nasal endoscopy revealed an exophytic papillomatous growth in the nasopharynx. MRI showed lesion arising from the nasopharyngeal surface of the soft palate. The lesion was free from the posterior pharyngeal wall. The patient was taken up for the procedure under general anaesthesia. The transoral approach was followed first. The tissue was taken for histopathological examination followed by a traction suture placed over uvula for better visualisation. Once exposed, coblation device was used transorally with 45 degree hopkins rod transorally. The tissue was ablated with coblation and coagulation settings of 9:5 respectively. The base was ablated too, to prevent further recurrence. Tonsillar pillar retractor was then used for better visualisation and exposure. The coblation was then continued. The tissue was removed transorally as much as possible then trans nasal approach was performed. Then, the same coblation device with the same setting was used but the nasal endoscope was changed to O degree Pediatric scope due to space constraints. The lesion was pushed upward with the help of yankaurs suction tip for better exposure and the remaining tissue was removed with the help of same coblation device. The lesion was excised completely and successfully with minimal blood loss. The operative area was confirmed with the 70Degree hopkins rod for complete removal of the lesion. Post operative recovery was uneventful. Combined transoral trans nasal coblation assisted approach is potential to be safer, easier and less invasive than uvulo palato pharyngoplasty in Pediatric age group specially, in the areas which are difficult to access like nasopharyngeal surface of the soft palate what we showed in this video.
Phaco in Phacomorphic Catarcact
videoExplains tips for performing phaco emulsification in a hyper mature cataract .
leadership (3)
Ravi N. Samy, MD, FACS
leadership
University of Cincinnati
- Director, Cochlear Implant and Auditory Brainstem Implant Program
- Program Director, Neurotology Fellowship
- Associate Professor, Department of Otolaryngology
Dr. Ravi Samy was born in Madras (now Chennai), India. He emigrated to the United States in 1973, at the age of 4. The first city in the US in which he lived was Canton, OH. After spending a few years in Connecticut during his father’s psychiatry residency, he moved to Wichita Falls, TX. He spent most of his formative years in Texas and considers himself a Texan. After graduating high school as co-valedictorian, Dr. Samy matriculated at Duke University. He graduated magna cum laude with a BS in Zoology in 1991. He then stayed on at Duke University School of Medicine and graduated in 1995. From 1995-2000, Dr. Samy was an intern and then a resident at Stanford University School of Medicine, where he developed a love for otology, neurotology, and skull base surgery. From 2000-2002, he was a fellow in Neurotology at the University of Iowa. After graduating, he was an Assistant Professor from 2002-2005 at UT-Southwestern Medical Center in Dallas, TX. Although he never wanted to leave Texas again, he was enamored with a phenomenal academic opportunity in the Department of Otolaryngology at the University of Cincinnati/Cincinnati Children’s Medical Center. He has been there for almost 8 years. He became an Associate Professor last year. During his time here, he has created an ACGME accredited, two-year Neurotology fellowship, one of only approximately 15 in the country. Dr. Samy serves not only as Program Director for the Neurotology Fellowship but also as the Director of the Cochlear Implant and Auditory Brainstem Implant program. His research interests include cochlear and auditory brainstem implantation as well as acoustic neuromas, neurofibromatosis type 2, facial nerve tumors, and other diseases and disorders of the lateral skull base. Finally, he is interested in using novel techniques and technologies to eradicate tumors, such as the use of surgical robotic systems or synthetic biology in the form of bacterial robotics systems. He is collaborating with researchers in India, including one of his former fellows, to incorporate these technologies and to enhance global health and increase collaboration between UC and international institutions, thus benefiting both US citizens and those of other nations.
Dr. Samy’s website, CiSurgeon.org provides information about Cochlear Implants, including FAQ, Cochlear Implant Surgery, preparation and more.
Rohan R. Walvekar, MD
leadership
University of Pittsburgh / VA Medical Center
- Assistant Professor in Head Neck Surgery
Rohan R. Walvekar, MD, earned his doctoral degree from the University of Mumbai. After graduating in 1998, he completed a residency in Otolaryngology and Head Neck Surgery at the TN Medical College & BYL Nair Charitable Hospital, Mumbai, India, with triple honors. Subsequently, he completed two head neck surgery fellowships, and trained at at the Tata Memorial Hospital, Mumbai, which is India's most prestigious cancer institute. After completing an Advanced Head Neck Oncologic Surgery fellowship at the University of Pittsburgh, he became an Assistant Professor in Head Neck Surgery within the Department of Otolaryngology Head Neck Surgery at the University of Pittsburgh/VA Medical Center, prior to joining the LSU Health Sciences Center in July 2008. His clinical interests are head neck surgery and salivary endoscopy. His research interests include evaluating prognostic markers and clinical outcomes of head and neck cancer therapy and treatment of salivary gland disorders.
Nitin Garg, MD
leadership
Wake Forest University School of Medicine
- Assistant Professor, Vascular & Endovascular Surgery
Dr. Nitin Garg is an Assistant Professor in Vascular & Endovascular Surgery at Wake Forest University School of Medicine in Winston Salem, North Carolina. He graduated from the prestigious All India Institute of Medical Sciences (AIIMS) in New Delhi and pursued a Master’s in Public Health at Johns Hopkins Bloomberg School of Public Health in Baltimore. Dr. Garg completed General Surgery internship and residency at Creighton University in Omaha and Vascular Surgery Fellowship at the Mayo Clinic in Rochester.
Dr. Garg has a strong interest in clinical education and firmly believes that the adequate training of the next generation of surgeons is the responsibility of the surgeons in practice. He also believes that education of patients is critical for their buy in into their own health. Dr. Garg’s clinical interests include complex arterial and venous reconstructions, using both open and endovascular (or hybrid) techniques.
management (1)
Zachary Salopek
management
- Chief Information Officer and Founder – The Physician’s Edge
Zachary Salopek was born in Pittsburgh, Pennsylvania and attended Indiana University of Pennsylvania for his undergraduate degree in Communications. While there he took on roles such as the director of the school news station and treasurer of the National Broadcasting Society.
Upon leaving IUP he got a job with CLASS (Community Living and Support Services) on their IT team. That experience helped him secure his next role working his way up the ladder in the St. Mary’s County Public School System. He eventually made it to be a Project Coordinator in charge of the wireless network for the entire county.
In his current role, Mr. Salopek is responsible for the overall planning, organizing, and execution of all digital marketing and IT functions for CSurgeries.
webinar (7)
Advanced Salivary Endoscopy: Challenging Cases Diagnosis & Treatment
webinar

The advanced course will assume a basic understanding of the procedure. It will include complex interventions including endoscopic and combined open (transoral and external procedures), complications and management of complications, approach to revision surgery, in-office procedures, advanced radiology, and will include case studies.
Meet the Course Directors!

Rohan R. Walvekar, MD
Assistant Professor in Head Neck Surgery
University of Pittsburgh/VA Medical Center
Rohan R. Walvekar, MD, earned his doctoral degree from the University of Mumbai. After graduating in 1998, he completed a residency in Otolaryngology and Head Neck Surgery at the TN Medical College & BYL Nair Charitable Hospital, Mumbai, India, with triple honors. Subsequently, he completed two head neck surgery fellowships, and trained at at the Tata Memorial Hospital, Mumbai, which is India's most prestigious cancer institute. After completing an Advanced Head Neck Oncologic Surgery fellowship at the University of Pittsburgh, he became an Assistant Professor in Head Neck Surgery within the Department of Otolaryngology Head Neck Surgery at the University of Pittsburgh/VA Medical Center, prior to joining the LSU Health Sciences Center in July 2008. His clinical interests are head neck surgery and salivary endoscopy. His research interests include evaluating prognostic markers and clinical outcomes of head and neck cancer therapy and treatment of salivary gland disorders.

Barry M Schaitkin, MD
Professor of Otolaryngology
UPMC Pittsburgh
Dr. Schaitkin specializes in the treatment of inflammatory and neoplastic conditions of the salivary glands. He practices at UPMC in the Department of Otolaryngology and is affiliated with UPMC branches all across the city of Pittsburgh. He completed his medical degree and residency at Pennsylvania State University College of Medicine.
Meet the Presenters!

Jolie Chang, MD
Associate Professor, Chief of Sleep Surgery and General Otolaryngology
University of California, San Francisco
Dr. Chang specializes in sleep apnea surgery and minimally invasive approaches to the salivary duct with sialendoscopy. She has interest in studying patient reported outcomes after sialendoscopy procedures.

Mark Marzouk, MD
Clinical Associate Professor of Otolaryngology - Head and Neck Surgery
SUNY Upstate Medical University
Dr. Marzouk completed his residency training in 2010 from the UPMC Department of Otolaryngology. He is currently the Division Chief of Head and Neck Oncologic Surgery in Syracuse. He is also the Associate Program Director of Residency Programs.
David W. Eisele, MD. FACS
Andelot Professor and Director - Department of Otolaryngology-Head and Neck Surgery
Johns Hopkins University School of Medicine
Dr. Eisele is the Past-President of the American Board of Otolaryngology- Head and Neck Surgery and a member of the NCCN Head and Neck Cancer Panel. He has served as a member of the Residency Review Committee for Otolaryngology, as Chair of the Advisory Council for Otolaryngology - Head and Neck Surgery for the American College of Surgeons, President of the American Head and Neck Society, and as Vice-President of the Triological Society. He served as President of the Maryland Society of Otolaryngology and is a former Governor of the American College of Surgeons.

M. Boyd Gillespie, MD, MSc, FACS
Professor and Chair
UTHSC Otolaryngology-Head and Neck Surgery
M. Boyd Gillespie is Professor and Chair of Otolaryngology-Head & Neck Surgery at University of Tennessee Health Science Center. He is a graduate of the Johns Hopkins University School of Medicine where he a completed residency and fellowship in Otolaryngology-Head & Neck Surgery. Dr. Gillespie earned a Masters in Clinical Research at the Medical University of South Carolina, and is board certified in Otolaryngology-Head and Neck Surgery and Sleep Medicine. He has published over 150 academic papers and is editor of the textbook Gland-Preserving Salivary Surgery: A Problem-Based Approach. He is a former Director of the American Board of Otolaryngology-Head & Neck Surgery (ABOHNS) and current member of the otolaryngology section of the Accreditation Council for Graduate Medical Education (ACGME).

M. Allison Ogden, MD FACS
Professor & Vice-Chair of Clinical Operations - Department of Otolaryngology
Washington University School of Medicine
Dr. Ogden is a Professor and Vice-Chair of Clinical Operations in the Department of Otolaryngology at Washington University School of Medicine. She graduated from the Washington University School of Medicine in 2002 and went on to complete her residency there as well in Otolaryngology in 2007. Her clinical interests include sialendoscopy, nasal obstructions, and hearling loss. In 2015 Dr. Ogden was listed in "Best Doctors in America", an honor that continues to this day.
Arjun S. Joshi, MD
Professor of Surgery
The George Washington University School of Medicine & Health Sciences
Arjun Joshi, MD is board-certified in Otolaryngology and Head & Neck surgery by both the American Board of Otolaryngology – Head and Neck Surgery and the Royal College of Physicians and Surgeons of Canada. Dr. Joshi received his medical degree from the State University of New York at Syracuse and completed his residency at The George Washington University Medical Center. His areas of expertise include: Head and Neck Cancer, Head and Neck Masses, Head and Neck Reconstruction, Thyroid and Parathyroid Surgery, and Salivary Endoscopy.

Henry T. Hoffman, MD
Professor of Otolaryngology / Professor of Radiation Oncology
University of Iowa Healthcare
Dr. Henry T. Hoffman is an ENT-otolaryngologist in Iowa City, Iowa and is affiliated with University of Iowa Hospitals and Clinics. He received his medical degree from University of California San Diego School of Medicine and has been in practice for more than 20 years.

David M. Cognetti, MD, FACS
Professor and Chair of Department of Otolaryngology-Head & Neck Surgery
Thomas Jefferson University
Dr. Cognetti received his BS in Biology from Georgetown University and his MD from the University of Pittsburgh School of Medicine. He completed a residency in Otolaryngology – Head and Neck Surgery at Thomas Jefferson University before completing a fellowship in Advanced Head and Neck Oncologic Surgery at the University of Pittsburgh Medical Center. Dr. Cognetti returned to Jefferson, his professional home, as faculty in 2008.

Christopher H. Rassekh, MD, FACS
Professor in Department of Otorhinolaryngology - Head & Neck Surgery / Director of Penn Medicine Sialendoscopy Program
University of Pennsylvania
Christopher H. Rassekh, MD is Professor of Clinical Otorhinolaryngology-Head and Neck Surgery at Penn Medicine. He is the Director of the Penn Medicine Sialendoscopy Program, which provides evaluation of and minimally invasive surgery for diseases that cause swelling of the salivary glands including obstructive diseases such as salivary stones, salivary duct strictures and tumors. Dr. Rassekh sees patients with head and neck tumors including cancers of the mouth, throat, voice box, salivary gland, thyroid and neck and also was a very early adopter of Transoral Robotic Surgery (TORS) for tumors and salivary gland diseases, and is an expert in cranial base surgery. He also is co-chair of the Airway Safety Committee at the Hospital of the University of Pennsylvania.
Covid-19 Impact on Anesthesia and Aero-Digestive Surgeries
webinar
Please join us for an interactive webinar on a variety of topics related to COVID 19. Organized by the Amrita Institute of Medical Sciences and Research Centre, Kochi, Kerala, India and moderated by Dr. Jayanthy Pavithran, Dr. Deepak Mehta, and Dr. Kishore Sandu, this panel will discuss the following topics:
1. Practical tips for endoscopy and use of powered instruments. | Presented by Dr. Deepak Mehta, Director, Pediatric Aerodigestive center and Dr. Shasidhar Tatavarthy, Senior consultant, Head, Ent Head Neck surgery Artemis Hospitals, Delhi
2. Psychiatry and C19. | Presented by Dr. Kusum Kathpalia (NY State)
3. Covid 19: An anesthetist’s view point from its pathogenesis to future airway interventions. | Presented by Dr. Patrick Schoettker, Medecin Chef- Anesthesia department. Lausanne University Hospital. Switzerland
4. Airway surgeries during Covid times. | Presented by Dr. Kishore Sandu, Medecin Chef, ORL department, Lausanne University Hospital. Switzerland.
5. Albatross Cases In Airway. | Presented by Dr. EV Raman , Consultant ENT Surgeon, Convenor, Children’s Airway and Swallowing Center ( CASC),Manipal Hospital, Bangalore and Dr.Rakesh Srivastava, Senior Consultant (Laryngologist, Sushrut Institute of Plastic Surgery & Super speciality Hospital, Lucknow, India.
This webinar is geared towards: airway surgeons (adult & pediatric), laryngologists, ENT, anesthesiologists and phoniatricians (SLP).
For more info on the CSurgeries webinar series, please go to www.csurgeries.com
The Future of Otology/Neurotology Surgery and Education in the Post-COVID Era
webinar
Join this interactive webinar with Drs. Ravi N. Samy (Cincinnati), Per Caye-Thomasen (Denmark), Sampath Rao (India), Alex Karkas (France), and James G. Naples (Boston). These faculty members in otology/neurotology will discuss their thoughts on the future of otologic surgery after the pandemic.
The panel will discuss topics such as decision-making, the state of elective surgery, telemedicine, and many others.
This webinar is the third installation of a series on surgery in the COVID 19 era, brought to you by CSurgeries. To access the previous recordings please go to: www.csurgeries.com
This webinar is sponsored by Grace Medical (http://www.gracemedical.com/)
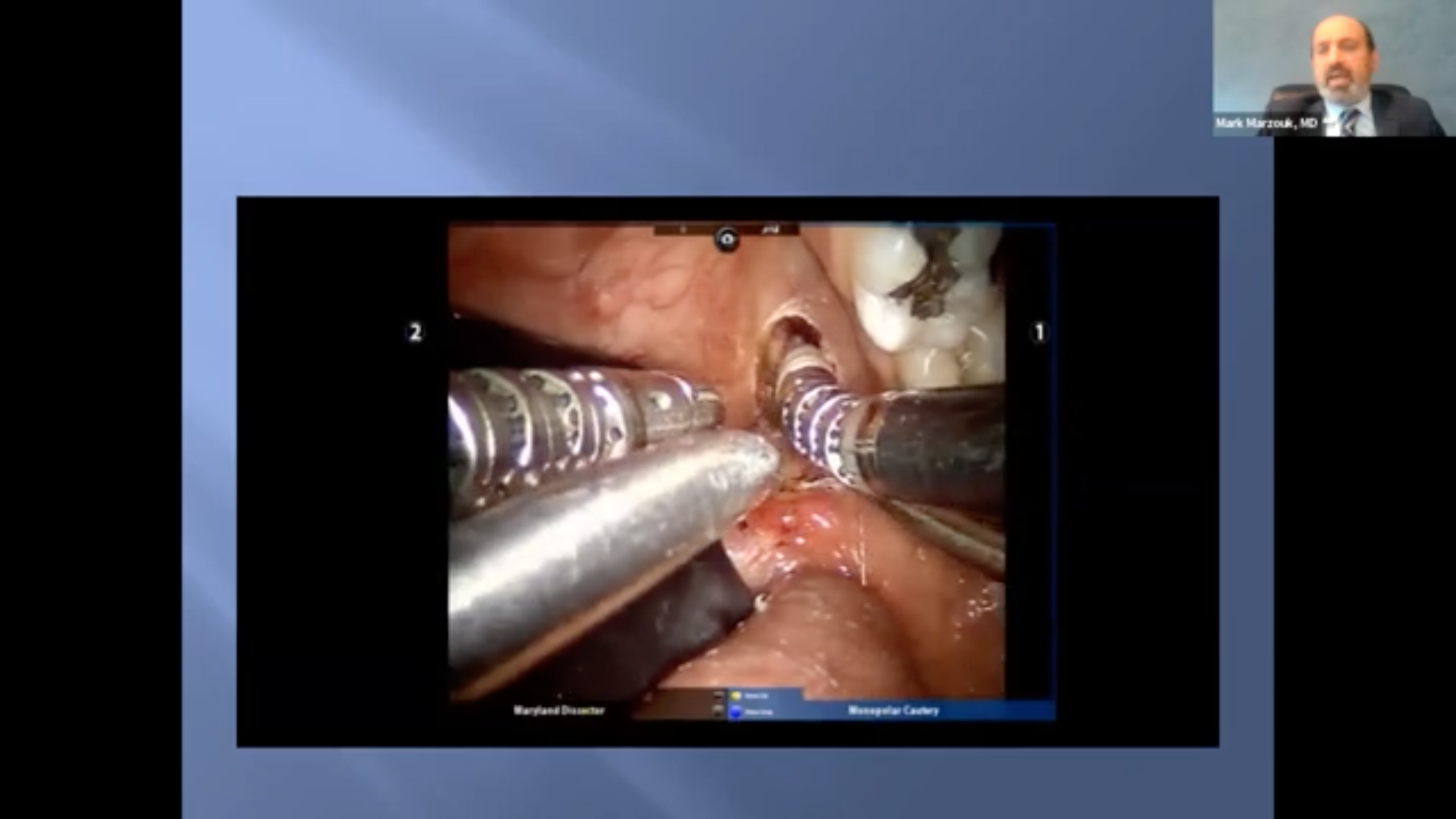
Salivary Interactive Case Study
webinar
Submit your own cases to be reviewed by our Salivary Surgery Experts, Dr. Rohan Walvekar and Dr. Barry Schaitkin. Cases will be selected prior to the session and those selected will be notified. Our experts, joined by guest panelists, will review the case details, provide their perspective, and go over alternative methods to consider when presented with a similar case.
If you feel uncomfortable submitting patient information, you can just bring the information to the session and present it directly to the experts. Here is what you need to have prepared when you join the webinar:
• Short patient history - medical and surgical
• Findings from images or scans - the actual images and scans are helpful too
• Any kind of operative images or videos that can help showcase the problem
• A question to pose to the expert panel


Assistant Professor in Head Neck Surgery
University of Pittsburgh/VA Medical Center
Rohan R. Walvekar, MD, earned his doctoral degree from the University of Mumbai. After graduating in 1998, he completed a residency in Otolaryngology and Head Neck Surgery at the TN Medical College & BYL Nair Charitable Hospital, Mumbai, India, with triple honors. Subsequently, he completed two head neck surgery fellowships, and trained at at the Tata Memorial Hospital, Mumbai, which is India's most prestigious cancer institute. After completing an Advanced Head Neck Oncologic Surgery fellowship at the University of Pittsburgh, he became an Assistant Professor in Head Neck Surgery within the Department of Otolaryngology Head Neck Surgery at the University of Pittsburgh/VA Medical Center, prior to joining the LSU Health Sciences Center in July 2008. His clinical interests are head neck surgery and salivary endoscopy. His research interests include evaluating prognostic markers and clinical outcomes of head and neck cancer therapy and treatment of salivary gland disorders.
Professor of Otolaryngology
UPMC Pittsburgh
Dr. Schaitkin specializes in the treatment of inflammatory and neoplastic conditions of the salivary glands. He practices at UPMC in the Department of Otolaryngology and is affiliated with UPMC branches all across the city of Pittsburgh. He completed his medical degree and residency at Pennsylvania State University College of Medicine.
What is Otolaryngology: More than Tonsils and Boogers
webinar
Come learn more about the jobs of Otolaryngologists (also known as ENT doctors!). We will discuss the breadth and depth of what ENT doctors cover with case descriptions. Medical students and residents of different levels will be on a panel to answer questions about the journey to and through Otolaryngology residency.

Otolaryngology Head and Neck Surgery / Resident Physician, PGY 5
Loyola University Medical Center
Dr Yang grew up in the arid and desert like climate of Eastern Washington before spending four years in rainy Seattle during her undergrad years, majoring in Neurobiology at the University of Washington. She then moved to sunny Southern California to complete her medical education at Loma Linda University School of Medicine. She is currently finishing her chief year of Otolaryngology Head and Neck Surgery residency at Loyola University Medical Center in Chicago, enjoying both life in the Windy City and surviving the cold winters. She recently matched to fellowship at Oregon Health and Science University in Facial Plastics and Reconstruction with Dr. Wax to specialize in microvascular reconstruction of complex head and neck defects. She is excited to return to the west coast and explore all the nature that Oregon has to offer.

Resident physician
University of Nebraska Medical Center
Steven is originally from San Diego, CA and attended the University of Notre Dame where he studied anthropology. He then earned a master's degree at Boston University and completed a year of service with Jesuit Volunteer Corps Northwest in Yakima, WA. Steven recently graduated from Loyola University Chicago Stritch School of Medicine and will be starting otolaryngology residency at the University of Nebraska Medical Center.
Medical Student
Loyola University Chicago Stritch School of Medicine
Alice is originally from San Jose, CA and attended UC Berkeley where she studied Molecular and Cell Biology as well as Nutrition. She is starting her fourth year at Loyola University Chicago Stritch School of Medicine, and preparing to apply for otolaryngology residency.

Resident
Loyola University Medical Center Otolaryngology Head and Neck Surgery Department
Dr. Sandelski grew up in Northwest Indiana, leaving the state for undergrad at the University of Michigan, and returning for medical school at Indiana University School of Medicine. She is in her second year at Loyola for ENT residency. She is undecided for plans after residency, with current interests in head and neck oncology and facial plastics and reconstruction.
Salivary Interactive Case Study: July
webinar
Submit your own cases to be reviewed by our Salivary Surgery Experts, Dr. Rohan Walvekar and Dr. Barry Schaitkin. Cases will be selected prior to the session and those selected will be notified. Our experts, joined by guest panelists, will review the case details, provide their perspective, and go over alternative methods to consider when presented with a similar case.
If you feel uncomfortable submitting patient information, you can just bring the information to the session and present it directly to the experts. Here is what you need to have prepared when you join the webinar:
• Short patient history - medical and surgical
• Findings from images or scans - the actual images and scans are helpful too
• Any kind of operative images or videos that can help showcase the problem
• A question to pose to the expert panel


Assistant Professor in Head Neck Surgery
University of Pittsburgh/VA Medical Center
Rohan R. Walvekar, MD, earned his doctoral degree from the University of Mumbai. After graduating in 1998, he completed a residency in Otolaryngology and Head Neck Surgery at the TN Medical College & BYL Nair Charitable Hospital, Mumbai, India, with triple honors. Subsequently, he completed two head neck surgery fellowships, and trained at at the Tata Memorial Hospital, Mumbai, which is India's most prestigious cancer institute. After completing an Advanced Head Neck Oncologic Surgery fellowship at the University of Pittsburgh, he became an Assistant Professor in Head Neck Surgery within the Department of Otolaryngology Head Neck Surgery at the University of Pittsburgh/VA Medical Center, prior to joining the LSU Health Sciences Center in July 2008. His clinical interests are head neck surgery and salivary endoscopy. His research interests include evaluating prognostic markers and clinical outcomes of head and neck cancer therapy and treatment of salivary gland disorders.
Professor of Otolaryngology
UPMC Pittsburgh
Dr. Schaitkin specializes in the treatment of inflammatory and neoplastic conditions of the salivary glands. He practices at UPMC in the Department of Otolaryngology and is affiliated with UPMC branches all across the city of Pittsburgh. He completed his medical degree and residency at Pennsylvania State University College of Medicine.
Salivary Interactive Case Study: August
webinar
Submit your own cases to be reviewed by our Salivary Surgery Experts, Dr. Rohan Walvekar and Dr. Barry Schaitkin. Cases will be selected prior to the session and those selected will be notified. Our experts, joined by guest panelists, will review the case details, provide their perspective, and go over alternative methods to consider when presented with a similar case.
If you feel uncomfortable submitting patient information, you can just bring the information to the session and present it directly to the experts. Here is what you need to have prepared when you join the webinar:
• Short patient history - medical and surgical
• Findings from images or scans - the actual images and scans are helpful too
• Any kind of operative images or videos that can help showcase the problem
• A question to pose to the expert panel


Assistant Professor in Head Neck Surgery
University of Pittsburgh/VA Medical Center
Rohan R. Walvekar, MD, earned his doctoral degree from the University of Mumbai. After graduating in 1998, he completed a residency in Otolaryngology and Head Neck Surgery at the TN Medical College & BYL Nair Charitable Hospital, Mumbai, India, with triple honors. Subsequently, he completed two head neck surgery fellowships, and trained at at the Tata Memorial Hospital, Mumbai, which is India's most prestigious cancer institute. After completing an Advanced Head Neck Oncologic Surgery fellowship at the University of Pittsburgh, he became an Assistant Professor in Head Neck Surgery within the Department of Otolaryngology Head Neck Surgery at the University of Pittsburgh/VA Medical Center, prior to joining the LSU Health Sciences Center in July 2008. His clinical interests are head neck surgery and salivary endoscopy. His research interests include evaluating prognostic markers and clinical outcomes of head and neck cancer therapy and treatment of salivary gland disorders.
Professor of Otolaryngology
UPMC Pittsburgh
Dr. Schaitkin specializes in the treatment of inflammatory and neoplastic conditions of the salivary glands. He practices at UPMC in the Department of Otolaryngology and is affiliated with UPMC branches all across the city of Pittsburgh. He completed his medical degree and residency at Pennsylvania State University College of Medicine.
news (1)
Introducing a Two-Part Sialendoscopy Series!
news
Brought to you by our partnership with Cook Medical, we are having a two-part series on Sialendoscopy. The sessions will feed into one another, the first covering basics like a review of instrumentation and set up, as well as some of the most basic interventions you will see.
The second session will assume a basic knowledge of the procedure and will deal with complex interventions including both endoscopic and combined open procedures, advanced radiology, and complication management for revision surgery and in-office procedures.
Meet the Course Directors!

Rohan R. Walvekar, MD
Assistant Professor in Head Neck Surgery
University of Pittsburgh/VA Medical Center
Rohan R. Walvekar, MD, earned his doctoral degree from the University of Mumbai. After graduating in 1998, he completed a residency in Otolaryngology and Head Neck Surgery at the TN Medical College & BYL Nair Charitable Hospital, Mumbai, India, with triple honors. Subsequently, he completed two head neck surgery fellowships, and trained at at the Tata Memorial Hospital, Mumbai, which is India's most prestigious cancer institute. After completing an Advanced Head Neck Oncologic Surgery fellowship at the University of Pittsburgh, he became an Assistant Professor in Head Neck Surgery within the Department of Otolaryngology Head Neck Surgery at the University of Pittsburgh/VA Medical Center, prior to joining the LSU Health Sciences Center in July 2008. His clinical interests are head neck surgery and salivary endoscopy. His research interests include evaluating prognostic markers and clinical outcomes of head and neck cancer therapy and treatment of salivary gland disorders.

Barry M Schaitkin, MD
Professor of Otolaryngology
UPMC Pittsburgh
Dr. Schaitkin specializes in the treatment of inflammatory and neoplastic conditions of the salivary glands. He practices at UPMC in the Department of Otolaryngology and is affiliated with UPMC branches all across the city of Pittsburgh. He completed his medical degree and residency at Pennsylvania State University College of Medicine.
Meet the Presenters!

Jolie Chang, MD
Associate Professor, Chief of Sleep Surgery and General Otolaryngology
University of California, San Francisco
Dr. Chang specializes in sleep apnea surgery and minimally invasive approaches to the salivary duct with sialendoscopy. She has interest in studying patient reported outcomes after sialendoscopy procedures.

Mark Marzouk, MD
Clinical Associate Professor of Otolaryngology - Head and Neck Surgery
SUNY Upstate Medical University
Dr. Marzouk completed his residency training in 2010 from the UPMC Department of Otolaryngology. He is currently the Division Chief of Head and Neck Oncologic Surgery in Syracuse. He is also the Associate Program Director of Residency Programs.
David W. Eisele, MD. FACS
Andelot Professor and Director - Department of Otolaryngology-Head and Neck Surgery
Johns Hopkins University School of Medicine
Dr. Eisele is the Past-President of the American Board of Otolaryngology- Head and Neck Surgery and a member of the NCCN Head and Neck Cancer Panel. He has served as a member of the Residency Review Committee for Otolaryngology, as Chair of the Advisory Council for Otolaryngology - Head and Neck Surgery for the American College of Surgeons, President of the American Head and Neck Society, and as Vice-President of the Triological Society. He served as President of the Maryland Society of Otolaryngology and is a former Governor of the American College of Surgeons.

M. Boyd Gillespie, MD, MSc, FACS
Professor and Chair
UTHSC Otolaryngology-Head and Neck Surgery
M. Boyd Gillespie is Professor and Chair of Otolaryngology-Head & Neck Surgery at University of Tennessee Health Science Center. He is a graduate of the Johns Hopkins University School of Medicine where he a completed residency and fellowship in Otolaryngology-Head & Neck Surgery. Dr. Gillespie earned a Masters in Clinical Research at the Medical University of South Carolina, and is board certified in Otolaryngology-Head and Neck Surgery and Sleep Medicine. He has published over 150 academic papers and is editor of the textbook Gland-Preserving Salivary Surgery: A Problem-Based Approach. He is a former Director of the American Board of Otolaryngology-Head & Neck Surgery (ABOHNS) and current member of the otolaryngology section of the Accreditation Council for Graduate Medical Education (ACGME).

M. Allison Ogden, MD FACS
Professor & Vice-Chair of Clinical Operations - Department of Otolaryngology
Washington University School of Medicine
Dr. Ogden is a Professor and Vice-Chair of Clinical Operations in the Department of Otolaryngology at Washington University School of Medicine. She graduated from the Washington University School of Medicine in 2002 and went on to complete her residency there as well in Otolaryngology in 2007. Her clinical interests include sialendoscopy, nasal obstructions, and hearling loss. In 2015 Dr. Ogden was listed in "Best Doctors in America", an honor that continues to this day.
Arjun S. Joshi, MD
Professor of Surgery
The George Washington University School of Medicine & Health Sciences
Arjun Joshi, MD is board-certified in Otolaryngology and Head & Neck surgery by both the American Board of Otolaryngology – Head and Neck Surgery and the Royal College of Physicians and Surgeons of Canada. Dr. Joshi received his medical degree from the State University of New York at Syracuse and completed his residency at The George Washington University Medical Center. His areas of expertise include: Head and Neck Cancer, Head and Neck Masses, Head and Neck Reconstruction, Thyroid and Parathyroid Surgery, and Salivary Endoscopy.

Henry T. Hoffman, MD
Professor of Otolaryngology / Professor of Radiation Oncology
University of Iowa Healthcare
Dr. Henry T. Hoffman is an ENT-otolaryngologist in Iowa City, Iowa and is affiliated with University of Iowa Hospitals and Clinics. He received his medical degree from University of California San Diego School of Medicine and has been in practice for more than 20 years.

David M. Cognetti, MD, FACS
Professor and Chair of Department of Otolaryngology-Head & Neck Surgery
Thomas Jefferson University
Dr. Cognetti received his BS in Biology from Georgetown University and his MD from the University of Pittsburgh School of Medicine. He completed a residency in Otolaryngology – Head and Neck Surgery at Thomas Jefferson University before completing a fellowship in Advanced Head and Neck Oncologic Surgery at the University of Pittsburgh Medical Center. Dr. Cognetti returned to Jefferson, his professional home, as faculty in 2008.