Search Results
We found 11 results for Emory University School of Medicine in video, leadership, webinar & news
video (3)
Submental Intubation
videoPresented is a case of submental intubation performed prior to maxillomandibular advancement for the treatment of obstructive sleep apnea. Submental intubation is a viable alternative to tracheostomy for cases in which nasal intubation is contraindicated (e.g. trauma), or uninterrupted access to the oral cavity is preferred. [1] Briefly, the technique consists of performing oral intubation, and then exteriorizing the endotracheal tube through a tract created from the floor of mouth to the submental triangle. At the end of the case, the tube can be passed into the oral cavity, returning to an oral intubation. Surgeon: Raj C. Dedhia, MD, MSCR, Department of Otolaryngology, Emory University School of Medicine Video Production: Clara Lee, MS4, Emory University School of Medicine
Endoscopic Nd:Yag and Bleomycin Injection for the management of a Hypopharyngeal Venous Malformation
videoVenous malformations (VM) are congenital lesions, frequently affecting the head and neck, with poor respect for tissue planes. Established treatments include observation, sclerotherapy, laser, and surgical resection.1 Lesions affecting the upper airways present unique challenge due to frequent unresectability and difficult access/exposure for alternative standard treatments. We describe our approach of standard endoscopic airway techniques for the administration of advanced treatment modalities including simultaneous laser and sclerotherapy for an extensive airway VM. Our patient is a 16-year-old female with an extensive multi-spatial VM with associated airway obstruction. The patient suffered from severe obstructive sleep apnea (OSA) and continuous positive airway pressure (CPAP) dependence as a result of airway compression. Direct laryngoscopy and bronchoscopy demonstrated extensive venous staining and large vascular channels of the hypopharynx. Lumenis Nd:Yag laser (Yokneam, Israel) via 550 micron fiber was passed under telescopic visualization. Treatment via previously described “polka dot” technique was performed (15W, 0.5 pulse duration) with immediate tissue response. The largest vascular channel was accessed via 25-gauge butterfly needle. Immediate return of blood following lesion puncture confirmed intralesional placement. Reconstituted bleomycin (1 U/kg; max dose = 15 U per treatment) was injected and hemostasis achieved with afrin pledgets. The patient was intubated overnight. She was extubated the next morning and advanced to a regular diet, discharging post-operative day two. Post-operative flexible laryngoscopy demonstrated significant improvement in the treatment areas, and follow up sleep study demonstrated sleep apnea resolution with liberation of her CPAP therapy.
Posterior Pharyngeal Flap for Large Gap Velopharyngeal Insufficiency
videoVelopharyngeal insufficiency (VPI) is a speech disorder characterized by inability for the palate (velum) to contact the posterior pharyngeal wall resulting in nasal air escape and subsequent speech abnormalities. All but the mildest cases are treated surgically, with technique chosen based on the closure pattern and gap size reserving the pharyngeal flap for the most severely affected patients. We present a 6-year old female with developmental delay and VPI with large (~60%) coronal pattern velopharyngeal gap subsequently deemed a candidate for posterior pharyngeal flap. Following Dingman mouthgag placement, the posterior wall is inspected and palpated ensuring no carotid medialization. The flap is designed and marked as wide and long as possible to reduce tension. Local injection wis performed. Using an angled needle tip Bovie, the flap was then elevated in the plane the prevertebral fascia to the level of the nasopharynx. The donor site is closed with simple interrupted 4.0 chromic sutures. The palatal mucosa is divided in a T-shaped fashion, without violating palatal musculature. The flap is inset with horizontal mattress sutures using 4.0 chromic. The nasal ports are inspected frequently to ensure adequate nasal airway patency. The palatal mucosa is reapproximated and any residual donor site closed. The patient is observed overnight, discharged home post-operative day 1, maintained on a soft diet for two weeks and abstains from speech therapy for 4 weeks to allow healing. Follow up demonstrated excellent healing well and VPI resolution on repeat speech sample.
leadership (2)
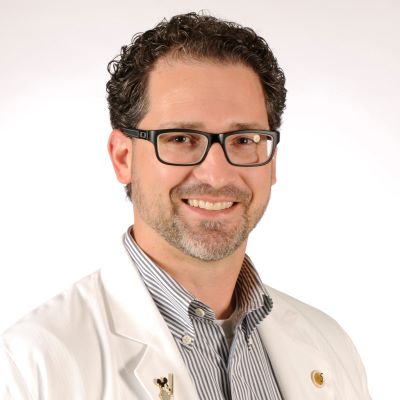
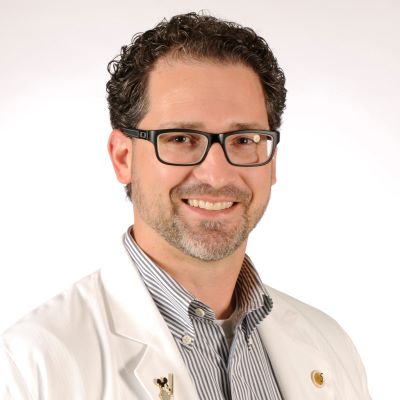
Michael Golinko, MD
leadership
University of Arkansas for Medical Sciences
- Medical Director of Craniofacial Program, Arkansas Children’s Hospital
- Assistant Professor of Plastic Surgery, UAMS
Dr. Michael Golinko, M.D., is a Board Certified General Surgeon with clinical interests in Craniofacial, Cleft & Paediatric Plastic Surgery. Dr. Golinko is also Board Eligible with the American Board of Plastic Surgery, and is licensed in the states of Arkansas, and Georgia. Currently, Dr. Golinko serves as one of the Medical Directors of Arkansas Children’s Hospital Craniofacial Program, and is Assistant Professor of Plastic Surgery at the University of Arkansas Medical Sciences.
Dr. Golinko received his M.D. degree from University of South Florida (USF) in 2004, preceded by a M.A. in Medical Anthropology from Universiteit van Amsterdam (UVA) in 2002, and a B.Sc. in Physics from Massachusetts Institute of Technology (MIT) in 1998.
Dr. Golinko’s professional training includes General Surgery residencies at State University of New York (SUNY) and New York University (NYU), as well as a residency in Plastic & Reconstructive Surgery at Emory University School of Medicine, and he most recently served as a Fellow in Craniofacial Surgery/Pediatric Plastic Surgery at New York University (NYU).
From 1998 to 2008, Dr. Golinko held medical research positions at MIT, Massachusetts General Hospital, and completed Post-Doctoral Research Fellowships in the Department of Surgery, Division of Wound Healing at both Columbia University and New York University.
Dr. Golinko has contributed extensively to numerous peer-reviewed publications, book chapters, and abstracts. Moreover, Dr. Golinko has travelled the world to deliver numerous presentations, co-chair lectures and conferences, and media appearances.
Dr. Golinko has been awarded and recognized for the following: Operation Smile Regan Fellowship Recipient (2012), National Institute of Health (NIH) Loan Repayment Program Recipient (2007 – 2009), and Columbia University College of Physicians & Surgeons, Department of Surgery, Startup Grant (2006).
In the spirit of a true leader, Dr. Golinko served as past-President and Mission Leader of Project World Health, Managing Trustee of the Barry Golinko Trust of the Jewish Communal Fund, past-Surgery Department Representative of the Committee on Interns and Residents (CIR) and currently was selected to participate in the Arkansas Children’s Hospital Physician Leadership Development course.
Dr. Golinko currently belongs to several professional societies as follows: American Cleft Palate-Craniofacial Association, American Association of Wound Care, American College of Surgeons, and the Southeastern Society Of Reconstructive Plastic Surgeons.
In 2016, Dr. Golinko served on the American Society of Maxillofacial Surgeons/Plastic Surgery Foundation Combined Pilot Research Grant Committee. In addition to his professional work, Dr. Golinko has generously donated his time and many talents to numerous volunteer and humanitarian efforts all over the world.
Michael M. Johns, III, MD
leadership
Emory University School of Medicine
- Director, Emory Voice Center
- Associate Professor
- Department of Otolaryngology
Dr. Johns is a graduate of Johns Hopkins School of Medicine. He completed his residency in Otolaryngology at the University of Michigan and trained as a research fellow through a National Institute of Health program. He then pursued a fellowship in laryngology and care of the professional voice at the Vanderbilt Voice Center at Vanderbilt University. Dr. Johns was awarded the highest honors during his academic career, including membership in Phi Beta Kappa and Alpha Omega Alpha medical honor society. He is the director of the Emory Voice Center at Emory University, pursing research, teaching and clinical care, with a specific interest in geriatric laryngology and the aging voice.
webinar (3)
Cleft Lip Revision: Tips and Tricks
webinar
Attendees will learn various tips and tricks to a successful cleft lip revision procedure. There will be a Q&A session to address common challenges and how to address them.
Course Directors

Larry Hartzell, MD FAAP is an Associate Professor of Otolaryngology Head and Neck Surgery at Arkansas Children’s Hospital. He is the Director of the Pediatric Otolaryngology fellowship. Dr Hartzell also has been the Cleft Team Director in Arkansas since 2012. He is passionate about international humanitarian mission work and dedicates much of his research efforts to cleft surgical and clinical care as well as velopharyngeal insufficiency. Dr Hartzell is actively involved in multiple academic societies and organizations including the AAO-HNS and ACPA.
Dr. Goudy is a professor at Emory University School of Medicine and the director of the division of otolaryngology at Children’s Healthcare in Atlanta. Dr. Goudy’s clinical job involves repair of craniofacial malformations including cleft lip, cleft palate, and Pierre Robin sequence, and he also participates in head and neck tumor resection and reconstruction.
Panelists


Dr. Leeper completed her residency training in Otolaryngology--Head & Neck Surgery at the Medical University of South Carolina in 2012 and fellowship training in Pediatric Otolaryngology at Arkansas Children's Hospital in 2014. She returned to the University of North Carolina - Chapel Hill in 2014 on faculty in the Department of Otolaryngology--Head & Neck Surgery. She is the current Fellowship Director and Medical Director of the Children's Cochlear Implant Center. She is married to Bradley and they have one daughter Sutton and a baby boy arriving this month.
Dr. Manlove joined Carle Foundation Hospital in 2016 as a fellowship trained cleft and craniomaxillofacial surgeon. She is the director of the cleft and craniofacial team at Carle. In 2018 she was name “Rising Star Physician” and that same year she also became the residency program director. Outside of work, she loves spending time with her family and she is an avid runner.


Dr. Kacmarynski is a Clinical Associate Professor in the Department of Otolaryngology-Head & Neck Surgery at the University of Iowa, working as a pediatric otolaryngologist and a cleft and craniofacial surgeon with co-directorship for the cleft and craniofacial team at the University of Iowa. Research focus is on biomedical collaborations with oral cleft and craniofacial surgical problems including craniofacial airway, tissue engineering solution development, outcomes research and patient-centered outcomes research collaboratives. I am excited about the long-term impacts of research leading very directly to significant improvements in our patients’ healing and growth.
Jordan Swanson, MD, MSc, is an attending surgeon in the Division of Plastic, Reconstructive and Oral Surgery at Children’s Hospital of Philadelphia with special clinical expertise in cleft, craniofacial, and pediatric plastic surgery. He holds the Linton A. Whitaker Endowed Chair in Plastic, Reconstructive and Oral Surgery.
Alveolar Bone Graft Surgery: Tips and Tricks
webinar
This webinar will focus on the surgical management of alveolar clefts with bone grafting and fistula closure. Our panel of experts will share various techniques and graft source materials including tips and tricks learned along the way. Our guest moderator will lead a panel discussion at the end of the session to discuss some of the controversies and key points in alveolar grafting.



| Dr. Larry Hartzell Director of Cleft Lip and Palate / Pediatric ENT Surgeon @ Arkansas Children's Hospital / University of Arkansas for Medical Sciences | Dr. Steven Goudy Professor / Director of Division of Otolaryngology @ Emory University School of Medicine / Children's Healthcare in Atlanta |
|---|---|
| Larry Hartzell, MD FAAP is an Associate Professor of Otolaryngology Head and Neck Surgery at Arkansas Children’s Hospital. He is the Director of the Pediatric Otolaryngology fellowship. Dr Hartzell also has been the Cleft Team Director in Arkansas since 2012. He is passionate about international humanitarian mission work and dedicates much of his research efforts to cleft surgical and clinical care as well as velopharyngeal insufficiency. Dr Hartzell is actively involved in multiple academic societies and organizations including the AAO-HNS and ACPA. | Dr. Goudy is a professor at Emory University School of Medicine and the director of the division of otolaryngology at Children’s Healthcare in Atlanta. Dr. Goudy’s clinical job involves repair of craniofacial malformations including cleft lip, cleft palate, and Pierre Robin sequence, and he also participates in head and neck tumor resection and reconstruction. |
| Travis T. Tollefson MD MPH FACS Professor & Director of Facial Plastic & Reconstructive Surgery @ University of California Davis | Mark E. Engelstad DDS, MD, MHI Associate Professor of Oral and Maxillofacial Surgery @ Oregon Health & Science University |
|---|---|
| Dr. Tollefson is a Professor and Director of Facial Plastic & Reconstructive Surgery at the University of California Davis, where he specializes in cleft and pediatric craniofacial care, facial reconstruction and facial trauma care. His interest in the emerging field of Global Surgery and improving surgical access in low-resource countries led him to complete an MPH at the Harvard School of Public Health. He helps lead the CMF arm of the AO-Alliance.org, whose goal is to instill AO principles in facial injuries in low resource settings. His current research focuses on clinical outcomes of patients with cleft lip-palate, facial trauma education in Africa, patterns of mandible fracture care, and patient reported outcomes in facial paralysis surgeries. He serves on the Board of Directors of the American Board of Otolaryngology- Head and Neck Surgery, American Academy of Facial Plastic Surgery, and is the Editor-In-Chief for Facial Plastic Surgery and Aesthetic Medicine journal. | Mark Engelstad is Associate Professor and Program Director of Oral and Maxillofacial surgery at Oregon Health & Science University in Portland, Oregon. His clinical practice focuses on the correction of craniofacial skeletal abnormalities, especially orthognathic surgery and alveolar bone grafting. |
| John K. Jones, MD, DMD Associate Professor in Oral and Maxillofacial Surgery @ University of Arkansas for Medical Sciences / Arkansas Children’ Hospital | David Joey Chang, DMD, FACS Associate Professor of Oral and Maxillofacial Surgery @ Tufts University/Tufts Medical Center |
|---|---|
| Dr. Jones has over 30 years of experience in the surgical management of cleft lip and palate with particular experience in the area of alveolar ridge grafting and corrective jaw surgery. He has been a member of the Cleft Lip and Palate Team at Arkansas Children’s Hospital for the last six years. During that time he has worked with Dr. Hartzell and his team to introduce and innovate new techniques, many from the realm of Oral and Maxillofacial Surgery and Dentistry, in the interest of improving outcomes for this most challenging patient population. | Dr. Chang is an associate professor at Tufts University School of Medicine and Tufts Medical Center. Dr. Chang is involved in the Cleft Team at Tufts Medical center since 2012. He also focuses on advanced bone grafting procedures, TMJ surgery, and nerve reconstruction. |
Cleft Primary and Revision Rhinoplasty: Tips and Tricks
webinar
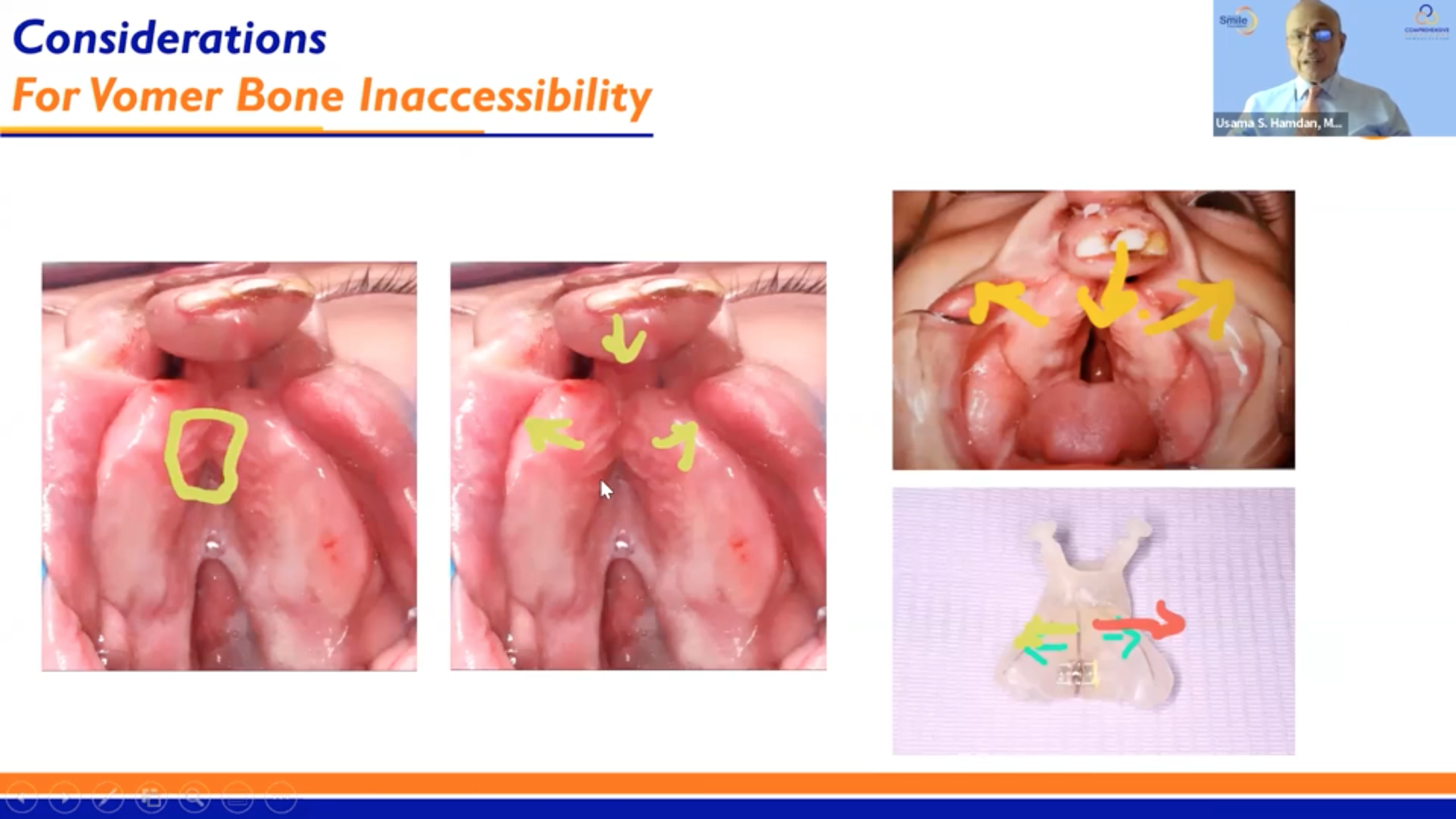
Tune in for the latest in our series on Cleft Surgery featuring Dr. Raj Vyas from UC Irvine and Dr. Usama Hamdan with the Global Smile Foundation. The discussion will focus on making sure that attendees know proper procedures as well as common complications and how to avoid them.
Larry Hartzell, MD FAAP is an Associate Professor of Otolaryngology Head and Neck Surgery at Arkansas Children’s Hospital. He is the Director of the Pediatric Otolaryngology fellowship. Dr Hartzell also has been the Cleft Team Director in Arkansas since 2012. He is passionate about international humanitarian mission work and dedicates much of his research efforts to cleft surgical and clinical care as well as velopharyngeal insufficiency. Dr Hartzell is actively involved in multiple academic societies and organizations including the AAO-HNS and ACPA.

Dr. Goudy is a professor at Emory University School of Medicine and the director of the division of otolaryngology at Children’s Healthcare in Atlanta. Dr. Goudy’s clinical job involves repair of craniofacial malformations including cleft lip, cleft palate, and Pierre Robin sequence, and he also participates in head and neck tumor resection and reconstruction.

Dr. Hamdan is President and Co-Founder of Global Smile Foundation, a 501C3 Boston-based non-profit foundation that provides comprehensive and integrated pro bono cleft care for underserved patients throughout the world. He has been involved with outreach cleft programs for over three decades. Dr. Hamdan is an Otolaryngologist/Facial Plastic Surgeon with former university appointments at Harvard Medical School, Tufts University School of Medicine and Boston University School of Medicine. For his philanthropic service to the people of Ecuador, he was awarded the Knighthood, “Al Merito Atahualpa” En El Grado De Caballero, by the President of Ecuador in March 2005. He received Honorary Professorship at Universidad de Especialidades Espíritu Santo, School of Medicine, in Ecuador on March 5, 2015 for his contributions in the field of Cleft Lip and Palate.

Dr. Vyas obtained his BS from Stanford and his MD from UCLA before completing integrated plastic surgery residency at Harvard and a fellowship in Craniofacial Surgery at NYU. He is an active clinician, scientist and educator with over 200 peer-reviewed publications and presentations, 20 book chapters, dozens of invited lectures, and multiple NIH and foundational grants. Dr. Vyas is passionate about advancing knowledge and skill for cleft care worldwide, partnering with Global Smile Foundation as both a clinician and Director of Research.

After completing a pediatric craniofacial fellowship at Boston Children’s Hospital, he joined the Division of Plastic and Reconstructive Surgery at Washington University in St. Louis 2011. He is Director of Craniofacial and Medical Director of the Operating Rooms at Saint Louis Children’s Hospital (SLCH). He treats patients with craniosynostosis or other craniofacial abnormalities (congenital or traumatic). He obtained a Master of Science in Clinical Investigation in May 2017 at Washington University to advance his ability to perform high quality clinical research and this program allows him to take advantage of the tremendous resources available for faculty and residents. His research focus is in craniofacial with particular interest in craniosynostosis and cleft lip and palate.

Dr. David Yates MD, DMD, FACS is passionate about serving children with Cranial and Facial deformities and Cleft Lip and Palate. He is a Board Certified Oral and Maxillofacial Surgeon and was recently awarded the inaugural “Physician of the Year” award by El Paso Children’s Hospital. He is the Division Chief of Cranial and Facial Surgery at El Paso Children’s Hospital and has been critical in bringing complex craniofacial surgery to the region. In addition to being a partner with High Desert Oral and Facial Surgery, he directs the craniofacial clinic at El Paso Children’s Hospital and the craniofacial clinic at Providence Memorial Hospital. He has also been integral in starting a clinic for children with Cleft Lip and Palate in Juarez, Mexico at the Hospital De La Familia (FEMAP). He is now happily settled with his wife and four kids serving the greater El Paso/Las Cruces/Juarez region.
news (3)
Meet our Presenters for Day 2!
news
The International Adult Airway Symposium is coming up this weekend! For more information view the itinerary or register here!
Dr. Vyvy Young
Associate Professor and the Associate Residency Program Director in the Department of Otolaryngology-Head and Neck Surgery
University of California – San Francisco
VyVy Young, MD, is an Associate Professor and the Associate Residency Program Director in the Department of Otolaryngology-Head and Neck Surgery at the University of California – San Francisco. Dr. Young received her undergraduate and medical degrees from the University of Louisville, in Louisville, Kentucky, where she also pursued her Otolaryngology training. She then completed a fellowship in Laryngology and Care of the Professional Voice at the University of Pittsburgh Voice Center. She currently serves the American Academy of Otolaryngology – Head and Neck Surgery as member of the Annual Meeting Program Committee and Executive Committee for ENThealth.org. She is immediate past-chair of the Voice Committee and the Women in Otolaryngology Communications Committee and was recently selected as chair of the Finance and Audit Committee of the American Broncho-Esophagological Association.

Justin Roe, PhD, FRCSLT
Clinical Service Lead - Speech and Language Therapy – National Centre for Airway Reconstruction
Imperial College Healthcare NHS Trust
Dr. Roe is a clinical-academic and service lead, specialising in dysphagia in benign and malignant head and neck disease. He leads the speech and language therapy service for the National Centre for Airway Reconstruction at Imperial College Healthcare NHS Trust and is a consultant and service lead at the Royal Marsden NHS Foundation Trust. He is an Honorary Clinical Senior Lecturer at Imperial College London and an investigator on a number of NIHR portfolio studies. He is currently on an NIHR Imperial Biomedical Research Centre/ Imperial Health Charity funded post-doctoral research fellowship. He is an elected council member for the British Laryngological Association and British Association of Head and Neck Oncologists.

Professor Anil Patel MBBS PhD FRCA
Clinical Anaesthetist / Chairman of Department of Anaesthesia
Royal National ENT & Eastman Dental Hospital
Professor Anil Patel graduated from University College London in 1991. He is a clinical anaesthetist and continues to develop and refine the largest experience of anaesthetising adult airway patients under general anaesthesia (> 6,000 procedures) in the UK, probably Europe and possibly the world. His research interests include all aspects of shared airway and difficult airway management. Professor Patel has been an invited speaker to over 300 national and international meetings in 38 countries. He has over 130+ peer reviewed publications, 25 book chapters, over 4,500 citations and an h-index of 25.

Robbi A. Kupfer, MD
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
University of Michigan
Dr. Kupfer is an Associate Professor of Otolaryngology-Head & Neck Surgery at the University of Michigan who specializes in Laryngology and Bronchoesophagology. She is the Program Director for the Laryngology Fellowship as well as the Otolaryngology Residency at the University of Michigan.

Alexander T. Hillel, MD, FACS
Associate Professor
Johns Hopkins University School of Medicine
Dr. Alexander Hillel is a Laryngologist, Residency Program Director, and Vice Director of Education in the Johns Hopkins Department of Otolaryngology – Head & Neck Surgery. His clinical practice and research centers on the treatment, prevention, and causes of laryngotracheal stenosis (LTS).

Dale Ekbom, MD
Associate Professor of Otolaryngology / Director of Voice Disorders/Laryngology
Mayo Clinic
Residency in Otolaryngology/Head and Neck Surgery at the University of Michigan with a fellowship in Laryngology/Care of the Professional Voice at Vanderbilt University Medical Center. Clinically specializing in voice, especially management of vocal fold paralysis, Zenker’s diverticulum and Cricopharyngeal muscle dysfunction, early laryngeal cancer, and airway compromise due to laryngeal, subglottic, and tracheal stenosis. Research interests include idiopathic subglottic stenosis and GPA with surgical and medical management of the airway, vocal fold paralysis, new injectables using Jellyfish collagen.

Dr. Ricky Thakrar
Consultant Chest Physician
University College London Hospital
Dr. Ricky Thakrar qualified in Medicine from Imperial College London. He trained in Respiratory Medicine at the Royal Brompton Hospital and completed his training in Northwest London. He was appointed to a three-year academic fellowship at UCL where his PhD examined state of the art bronchoscopy techniques for managing cancers arising in central airways and lung. He is a Consultant in Thoracic Medicine and his main interests are in interventional bronchoscopy procedures (laser resection, airway stenting, cryotherapy, photodynamic therapy and brachytherapy) for pre-malignant and malignant disease of the tracheobronchial tree.

Dr. Michael Rutter
Director of the Aerodigestive Center
Cincinnati Children's Hospital
Dr. Rutter is an ENT surgeon specializing in pediatric otolaryngology with an emphasis on airway problems in children, adolescents and young adults. His interests include tracheal reconstruction and complex airway surgery. Always a problem-solver, he strives to involve the patient in their own care by having them help evaluate the issue and then craft a solution together. He was drawn to his career by the challenge and highly individualized nature of pediatric airway problems and management. Dr. Rutter enjoys working in a multidisciplinary team setting and focusing on coordinated care for complex childhood airway conditions. He was honored to receive the 2016 Gabriel Frederick Tucker Award from the American Laryngological Association, and the 2018 Sylvan Stool Teaching Award from the Society for Ear Nose and Throat Advancement in Children (SENTAC). These awards are for his contributions to the field of pediatric laryngology. In addition to caring for patients, he is also dedicated to his research trying to find improvements in airway management.

Christopher T. Wootten, MD, MMHC
Director, Pediatric Otolaryngology—Head and Neck Surgery
Vanderbilt University Medical Center
Dr. Wootten has a longstanding interest in surgical management of congenital and acquired airway disorders. To better equip himself to lead the Pediatric ENT service through expansion, evolution of practice models, and differentiation into multidisciplinary care, Dr. Wootten obtained a Masters of Management in Health Care at Vanderbilt’s Owen School of Business in 2017. Areas of his professional research emphasis include airway obstruction in children and adults and aerodigestive care. He innovates minimally invasive surgical techniques in the head and neck. Dr. Wootten is actively investigating the role of eosinophil and mast cell-based inflammation in the pediatric larynx.

Karla O'Dell, M.D.
Assistant Professor / Co-director
USC Voice Center, Caruso Department of Otolaryngology Head and Neck Surgery @ University of Southern California / USC Center for Airway Intervention and Reconstruction
Karla O’Dell, MD, specializes in head and neck surgery and disorders of the voice, airway and swallowing. She is cofounder and codirector of the USC Airway Intervention & Reconstruction Center (USC Air Center).

Jeanne L. Hatcher, MD, FACS
Co-Director of the Emory Voice Center and Associate Professor of Otolaryngology
Emory University School of Medicine
Dr. Hatcher has been at Emory since 2014 after completing her laryngology fellowship with Dr. Blake Simpson; she specializes in open and endoscopic airway surgery as well as voice disorders. Dr. Hatcher is a member of the ABEA and post-graduate member of the ALA and also serves on the Ethics and Voice Committees for the American Academy of Otolaryngology Head and Neck Surgery.

Mr. Lee Aspland
Patient / Freelance Artist
Lee Aspland Photography
Lee Aspland is a photographer, author and mindful practitioner who creates photography that reflects his feelings about living in such a glorious world. He specializes in Mindful Photography, capturing a fleeting feeling or thought, a hope or fear, a frozen single moment in time.

Gemma Clunie, MSc, BA (Hon), MRCSLT
Clinical Specialist Speech-Language Pathologist (Airways/ENT) and HEE/NIHR Clinical Doctoral Research Fellow
Imperial College Healthcare NHS Trust/ Imperial College London, Department of Surgery & Cancer
Gemma is a Clinical Specialist Speech and Language Therapist with an interest in voice and swallowing disorders that is particularly focused on the benign ENT, head and neck, respiratory and critical care populations. Gemma is a current NIHR/HEE Clinical Doctoral Research Fellow at Imperial College London. Her PhD studies focus on the voice and swallowing difficulties of airway stenosis patients. She is based at Charing Cross Hospital in London where she has worked for the last six years as part of the National Centre for Airway Reconstruction, Europe’s largest centre for the management of airway disorders.

Niall C. Anderson, CPsychol, MSc, BSc
Lead Psychologist (formerly Respiratory Highly Specialist Health Psychologist)
Bart's Health NHS Trust (formerly Central & North West London NHS Foundation Trust)
Niall is a HCPC Registered & BPS Chartered Practitioner Health Psychologist, and BPS RAPPS Registered Supervisor. Niall has specialist experience of working within healthcare systems with people with long-term health conditions at all system levels to support physical, psychological and social wellbeing. Niall worked in the Airway Service at Charing Cross Hospital (London, UK) between January-December 2021 in order to develop and implement the Airway Psychology Service.
Introducing our presenters for the upcoming Cleft Lip Revision webinar!
news
This webinar comes as the latest in a long line of installments dealing with the Cleft Palate. In this session, attendees will learn various tips and tricks to a successful cleft lip revision procedure. There will be a Q&A session to discuss common challenges and how to address them.
Meet the Course Directors

Director of Cleft Lip and Palate / Pediatric ENT Surgeon
Arkansas Children's Hospital / University of Arkansas for Medical Sciences
Larry Hartzell, MD FAAP is an Associate Professor of Otolaryngology Head and Neck Surgery at Arkansas Children’s Hospital. He is the Director of the Pediatric Otolaryngology fellowship. Dr Hartzell also has been the Cleft Team Director in Arkansas since 2012. He is passionate about international humanitarian mission work and dedicates much of his research efforts to cleft surgical and clinical care as well as velopharyngeal insufficiency. Dr Hartzell is actively involved in multiple academic societies and organizations including the AAO-HNS and ACPA.
Professor / Director of Division of Otolaryngology
Emory University School of Medicine / Children's Healthcare in Atlanta
Dr. Goudy is a professor at Emory University School of Medicine and the director of the division of otolaryngology at Children’s Healthcare in Atlanta. Dr. Goudy’s clinical job involves repair of craniofacial malformations including cleft lip, cleft palate, and Pierre Robin sequence, and he also participates in head and neck tumor resection and reconstruction.
Meet the Presenters


Associate Professor of Department of Otolaryngology--Head & Neck Surgery, Division of Pediatric Otolaryngology
University of North Carolina - Chapel Hill
Dr. Leeper completed her residency training in Otolaryngology--Head & Neck Surgery at the Medical University of South Carolina in 2012 and fellowship training in Pediatric Otolaryngology at Arkansas Children's Hospital in 2014. She returned to the University of North Carolina - Chapel Hill in 2014 on faculty in the Department of Otolaryngology--Head & Neck Surgery. She is the current Fellowship Director and Medical Director of the Children's Cochlear Implant Center. She is married to Bradley and they have one daughter Sutton and a baby boy arriving this month.
Residency Program Director / Director Cleft and Craniofacial Team
Carle Foundation Hospital
Dr. Manlove joined Carle Foundation Hospital in 2016 as a fellowship trained cleft and craniomaxillofacial surgeon. She is the director of the cleft and craniofacial team at Carle. In 2018 she was name “Rising Star Physician” and that same year she also became the residency program director. Outside of work, she loves spending time with her family and she is an avid runner.


Associate Professor - Craniofacial Abnormalities & Pediatric Otolaryngology / Co-Director of Cleft and Craniofacial Team
University of Iowa Hospitals & Clinics
Dr. Kacmarynski is a Clinical Associate Professor in the Department of Otolaryngology-Head & Neck Surgery at the University of Iowa, working as a pediatric otolaryngologist and a cleft and craniofacial surgeon with co-directorship for the cleft and craniofacial team at the University of Iowa. Research focus is on biomedical collaborations with oral cleft and craniofacial surgical problems including craniofacial airway, tissue engineering solution development, outcomes research and patient-centered outcomes research collaboratives. I am excited about the long-term impacts of research leading very directly to significant improvements in o
Linton Whitaker Endowed Chair in Craniofacial Surgery
Children’s Hospital of Philadelphia, Division of Plastic Surgery
Jordan Swanson, MD, MSc, is an attending surgeon in the Division of Plastic, Reconstructive and Oral Surgery at Children’s Hospital of Philadelphia with special clinical expertise in cleft, craniofacial, and pediatric plastic surgery. He holds the Linton A. Whitaker Endowed Chair in Plastic, Reconstructive and Oral Surgery.
Dr. Sean Evans: Crafting Surgical Videos for the Digital Generation
news
Dr. Sean Evans is a pediatric otolaryngologist at Children’s Healthcare of Atlanta and an Assistant Professor at the Department of Otolaryngology - Head and Neck Surgery of Emory University School of Medicine. His areas of expertise include microtia, cleft and speech surgery, vascular anomalies, and endoscopic ear surgery.
Dr. Evans started creating content for CSurgeries in 2020 after the platform sparked his interest as a ‘one stop shop’ for high quality surgical video content that could be readily reviewed, “As a resident and trainee, I desired high quality surgical videos to expound my understanding of complex surgical techniques that I would read about in surgical texts.”
Dr. Evans finds the process of creating surgical videos very straightforward as it involves just a few steps, “I review my surgical cases for any less common or more interesting cases that may be beneficial for others to learn from. I record the surgery and upload it to my laptop. I then use iMovie to edit the videos into the ‘need to know’ steps and create an audio voiceover to describe what is happening on screen. After this, it is typically submission ready.“
While he occasionally encounters minor challenges in completing his videos due to his busy schedule, Dr. Evans shares that he finds motivation by looking back to his trainee days.
“Remembering back to when I was a trainee though, I’m re-invigorated to move forward with the creation process. I also try to find the time to do it in one sitting. As much is asked of us as academic surgeons, I find the best way to tackle the project is to do as much as possible in the initial editing.”
The process of producing surgical videos has paid off not just for Dr. Evans but also his mentees.
“My learners routinely comment that they use my content for surgical case prep which is amazing to hear!” He notes, adding, “Each successful publication on CSurgeries has motivated me to create more content. They are good for a young physician like myself trying to gain traction in the field and look good as well come promotion time through an organization.”
For surgeons and medical students who would like to create surgical videos on CSurgeries, he urges them to take on the challenge, “The first step is the hardest. Find a case you’re proud of, think of what others can learn from, and want to share and sit down and do it!”
Dr. Evans envisions that surgical videos will play more of a role in medical education especially for a generation who grew up in an age where information is just one tap away, “With evolving modalities for recording and editing videos and graphics, I feel the future of surgical education is becoming more digitized. CSurgeries will be poised to be a leader in this space as a new generation of physicians who grew up on their devices searches for alternatives to classic texts and papers for elucidating surgical technique and efficiency.”